Download Annual Physical Examination Template
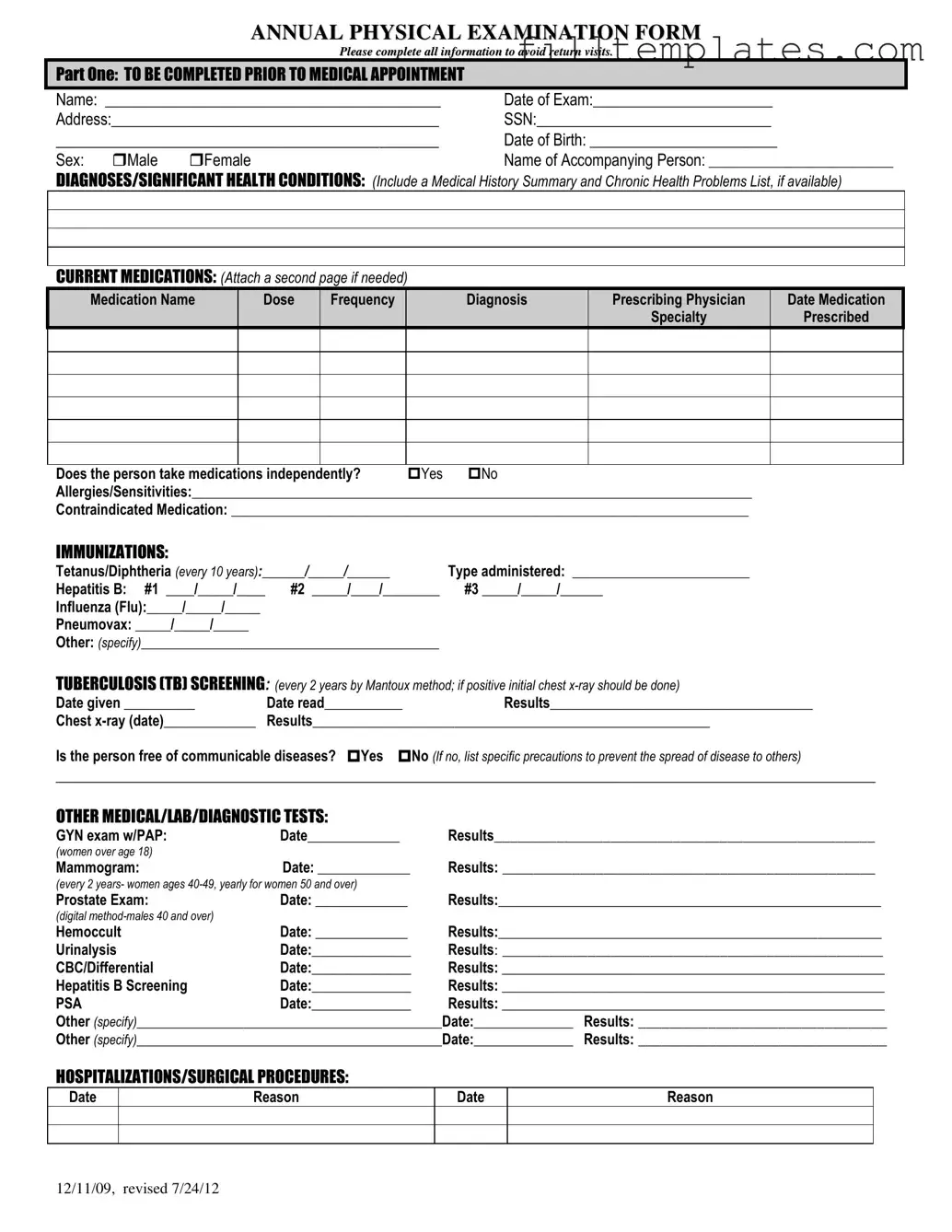
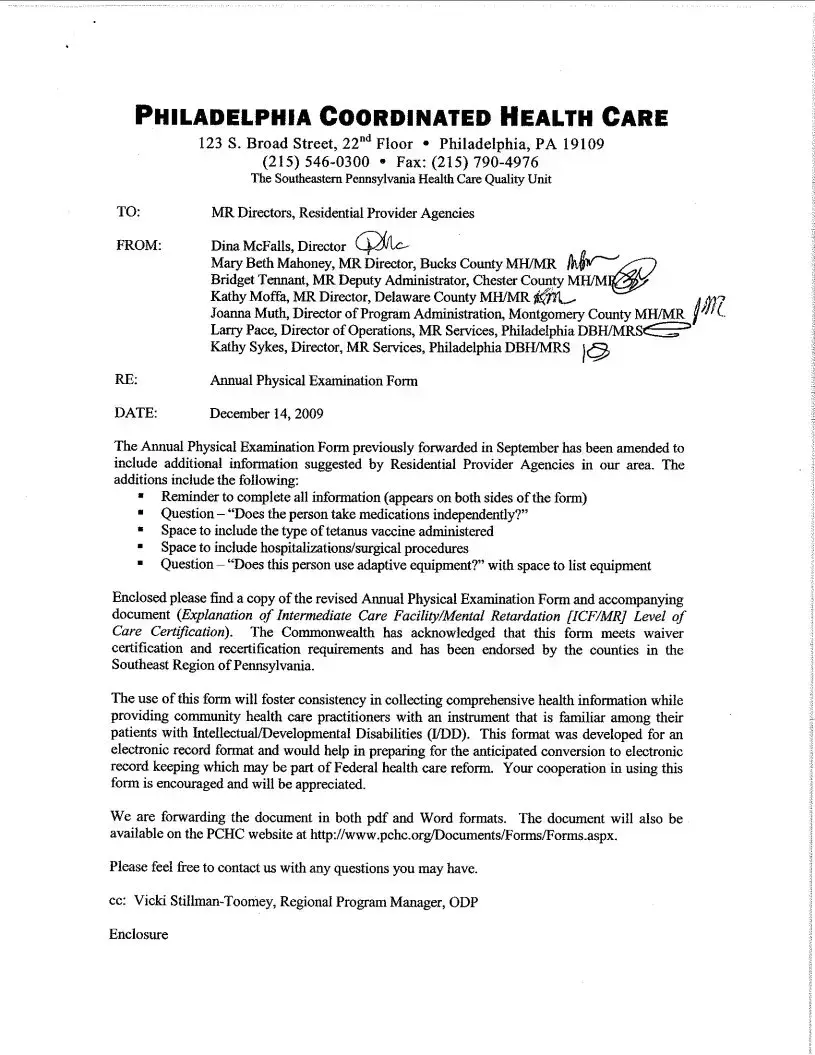
The Annual Physical Examination form is a crucial document designed to streamline the process of gathering essential health information prior to a medical appointment. This comprehensive form requires patients to provide personal details such as their name, date of birth, and contact information. It also prompts individuals to disclose any significant health conditions, current medications, and allergies, ensuring that healthcare providers have a complete understanding of their medical history. Immunization records are also included, detailing vaccinations like Tetanus, Hepatitis B, and Influenza, which are vital for preventive care. The form further addresses tuberculosis screening and various diagnostic tests, such as GYN exams, mammograms, and prostate exams, tailored to specific age groups and genders. Additionally, it encompasses a general physical examination section, where vital signs and evaluations of various body systems are recorded. This thorough approach not only aids in effective diagnosis and treatment but also emphasizes the importance of proactive health management.
Key takeaways
Completing the Annual Physical Examination form accurately is crucial for ensuring a smooth medical appointment. Here are key takeaways to consider:
- Complete All Sections: Fill out every part of the form to avoid delays or the need for return visits.
- Provide Accurate Personal Information: Include your name, date of birth, and contact details to ensure proper identification.
- List Current Medications: Detail all medications you are currently taking, including dosage and prescribing physician, to inform your healthcare provider.
- Document Allergies: Clearly state any allergies or sensitivities to medications to prevent adverse reactions during treatment.
- Update Immunization Records: Include dates and types of immunizations received, as this information is essential for preventive care.
- Health History is Important: Summarize significant health conditions and previous hospitalizations to give your physician a complete picture of your health.
- Be Honest About Symptoms: Indicate any current health issues or symptoms you are experiencing to guide the examination process.
- Review Recommendations: After your exam, pay attention to any health maintenance recommendations provided by your physician.
- Sign and Date the Form: Ensure that the form is signed and dated by both you and your physician to validate the information provided.
By following these guidelines, individuals can facilitate a more effective and efficient annual physical examination process.
Guide to Writing Annual Physical Examination
Completing the Annual Physical Examination form is an essential step to ensure that your medical appointment runs smoothly. By providing accurate and thorough information, you help healthcare providers understand your medical history and current health status. This process is straightforward, and following the steps below will guide you through filling out the form correctly.
- Personal Information: Fill in your name, date of exam, address, Social Security Number (SSN), date of birth, and sex. If someone is accompanying you, include their name as well.
- Medical History: List any significant health conditions and diagnoses. If you have a medical history summary or a list of chronic health problems, attach it to the form.
- Current Medications: Write down all medications you are currently taking, including the name, dose, frequency, diagnosis, prescribing physician, and specialty. Indicate whether you take these medications independently and note any allergies or contraindicated medications.
- Immunizations: Document your immunization history, including dates for Tetanus/Diphtheria, Hepatitis B, Influenza, Pneumovax, and any other relevant vaccines.
- Tuberculosis Screening: Record the date given and date read for your TB screening. Include the results and any chest x-ray information if applicable.
- Other Medical Tests: List any other medical, lab, or diagnostic tests you have had, along with their dates and results. This may include GYN exams, mammograms, prostate exams, and more.
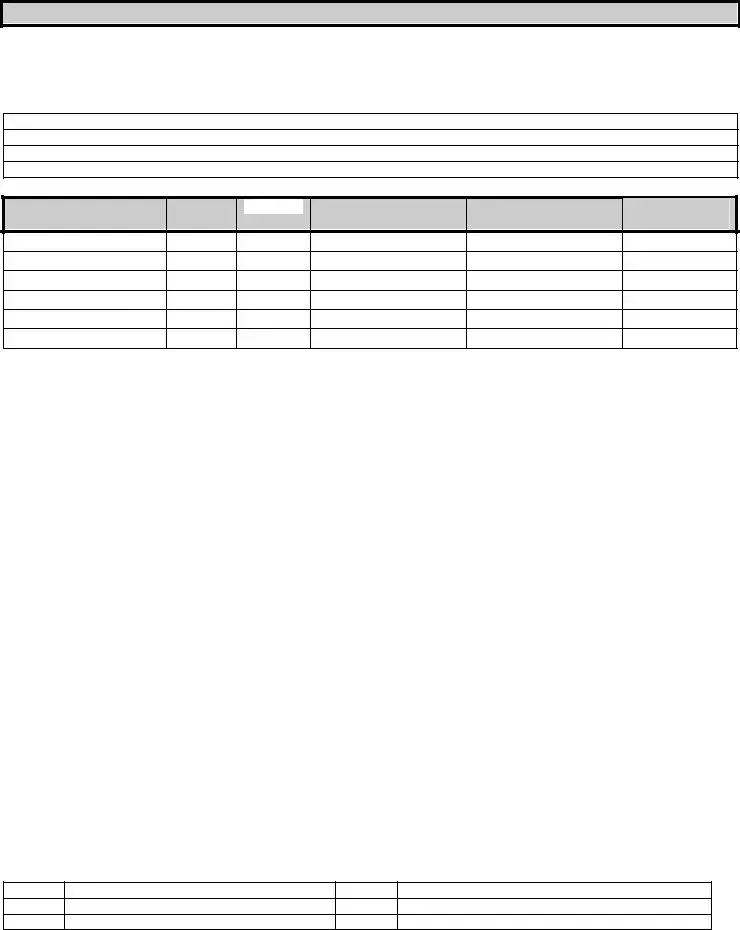
- General Physical Examination: Fill in your blood pressure, pulse, respirations, temperature, height, and weight.
- Evaluation of Systems: Indicate whether normal findings were observed for each system listed. Provide comments or descriptions where necessary.
- Vision and Hearing Screening: Note if further evaluation is recommended for either vision or hearing.
- Additional Comments: Review your medical history summary and note any changes to medications. Include recommendations for health maintenance, diet, and any special instructions.
- Activity Limitations: Specify if there are any limitations or restrictions on activities, and indicate whether adaptive equipment is used.
- Health Changes: Note any changes in health status from the previous year and indicate if specialty consultations are recommended.
- Physician Information: Print the name of your physician, sign the form, and provide the physician’s address and phone number.
Browse Other PDFs
High School Transcript - Allows students to discuss their educational journey with potential employers.
When requesting a Recommendation Letter form, it's important to provide the referrer with all necessary information to make their endorsement impactful. This form serves as a critical tool in showcasing an individual's strengths and suitability for a position or academic opportunity, ensuring that evaluators have a comprehensive understanding of the candidate’s qualifications. For more details on how to effectively utilize these forms, you can visit smarttemplates.net.
Correction Deed California - The affidavit reinforces the significance of accurate record-keeping in legal affairs.
Pdf Southern California Edison Bill Template - The form highlights your service account number to streamline payment processing.
Form Preview Example

ANNUAL PHYSICAL EXAMINATION FORM
Please complete all information to avoid return visits.
PART ONE: TO BE COMPLETED PRIOR TO MEDICAL APPOINTMENT
Name: ___________________________________________ |
Date of Exam:_______________________ |
Address:__________________________________________ |
SSN:______________________________ |
_____________________________________________ |
Date of Birth: ________________________ |
||
Sex: |
Male |
Female |
Name of Accompanying Person: __________________________ |
DIAGNOSES/SIGNIFICANT HEALTH CONDITIONS: (Include a Medical History Summary and Chronic Health Problems List, if available)
CURRENT MEDICATIONS: (Attach a second page if needed)
Medication Name |
Dose |
Frequency |
Diagnosis |
Prescribing Physician |
Date Medication |
|
|
|
|
Specialty |
Prescribed |
Does the person take medications independently? |
Yes |
No |
Allergies/Sensitivities:_______________________________________________________________________________ |
||
Contraindicated Medication: _________________________________________________________________________
IMMUNIZATIONS:
Tetanus/Diphtheria (every 10 years):______/_____/______ |
Type administered: _________________________ |
|
Hepatitis B: #1 ____/_____/____ |
#2 _____/____/________ |
#3 _____/_____/______ |
Influenza (Flu):_____/_____/_____ |
|
|
Pneumovax: _____/_____/_____ |
|
|
Other: (specify)__________________________________________ |
|
|
TUBERCULOSIS (TB) SCREENING: (every 2 years by Mantoux method; if positive initial chest |
||
Date given __________ |
Date read___________ |
Results_____________________________________ |
Chest |
Results________________________________________________________ |
|
Is the person free of communicable diseases? Yes No (If no, list specific precautions to prevent the spread of disease to others)
_________________________________________________________________________________________________________
OTHER MEDICAL/LAB/DIAGNOSTIC TESTS:
GYN exam w/PAP: |
Date_____________ |
Results_________________________________________________ |
(women over age 18) |
|
|
Mammogram: |
Date: _____________ |
Results: ________________________________________________ |
(every 2 years- women ages
Prostate Exam: |
Date: _____________ |
Results:______________________________________________________ |
|
(digital |
|
|
|
Hemoccult |
Date: _____________ |
Results:______________________________________________________ |
|
Urinalysis |
Date:______________ |
Results: _________________________________________________ |
|
CBC/Differential |
Date:______________ |
Results: ______________________________________________________ |
|
Hepatitis B Screening |
Date:______________ |
Results: ______________________________________________________ |
|
PSA |
Date:______________ |
Results: ______________________________________________________ |
|
Other (specify)___________________________________________Date:______________ |
Results: ________________________________ |
||
Other (specify)___________________________________________Date:______________ |
Results: ________________________________ |
||
HOSPITALIZATIONS/SURGICAL PROCEDURES:
Date
Reason
Date
Reason
12/11/09, revised 7/24/12
PART TWO: GENERAL PHYSICAL EXAMINATION
|
|
|
|
|
Please complete all information to avoid return visits. |
|
|
|
|
|
Blood Pressure:______ /_______ Pulse:_________ |
Respirations:_________ Temp:_________ Height:_________ |
Weight:_________ |
||||
|
|
EVALUATION OF SYSTEMS |
|
|
|
|
||
|
|
|
|
|
|
|
||
|
|
System Name |
|
Normal Findings? |
Comments/Description |
|
||
|
|
Eyes |
|
Yes |
No |
|
|
|
|
|
Ears |
|
Yes |
No |
|
|
|
|
|
Nose |
|
Yes |
No |
|
|
|
|
|
Mouth/Throat |
|
Yes |
No |
|
|
|
|
|
Head/Face/Neck |
|
Yes |
No |
|
|
|
|
|
Breasts |
|
Yes |
No |
|
|
|
|
|
Lungs |
|
Yes |
No |
|
|
|
|
|
Cardiovascular |
|
Yes |
No |
|
|
|
|
|
Extremities |
|
Yes |
No |
|
|
|
|
|
Abdomen |
|
Yes |
No |
|
|
|
|
|
Gastrointestinal |
|
Yes |
No |
|
|
|
|
|
Musculoskeletal |
|
Yes |
No |
|
|
|
|
|
Integumentary |
|
Yes |
No |
|
|
|
|
|
Renal/Urinary |
|
Yes |
No |
|
|
|
|
|
Reproductive |
|
Yes |
No |
|
|
|
|
|
Lymphatic |
|
Yes |
No |
|
|
|
|
|
Endocrine |
|
Yes |
No |
|
|
|
|
|
Nervous System |
|
Yes |
No |
|
|
|
|
|
VISION SCREENING |
|
Yes |
No |
Is further evaluation recommended by specialist? |
Yes |
No |
|
|
HEARING SCREENING |
|
Yes |
No |
Is further evaluation recommended by specialist? |
Yes |
No |
|
|
ADDITIONAL COMMENTS: |
|
|
|
|
|
|
|
|
|
|
|
|
|
||
|
|
Medical history summary reviewed? |
Yes |
No |
|
|
||
Medication added, changed, or deleted: (from this appointment)__________________________________________________________
Special medication considerations or side effects: ________________________________________________________________
Recommendations for health maintenance: (include need for lab work at regular intervals, treatments, therapies, exercise, hygiene, weight control, etc.)
___________________________________________________________________________________________________________
Recommendations for manual breast exam or manual testicular exam: (include who will perform and frequency)____________________
___________________________________________________________________________________________________________
Recommended diet and special instructions: ____________________________________________________________________
Information pertinent to diagnosis and treatment in case of emergency:
___________________________________________________________________________________________________________
Limitations or restrictions for activities (including work day, lifting, standing, and bending): No Yes (specify)
___________________________________________________________________________________________________________ |
|||
Does this person use adaptive equipment? |
No |
Yes (specify):________________________________________________ |
|
Change in health status from previous year? No |
Yes (specify):_________________________________________________ |
||
This individual is recommended for ICF/ID level of care? (see attached explanation) Yes |
No |
||
Specialty consults recommended? No |
Yes (specify):_________________________________________________________ |
||
Seizure Disorder present? No Yes (specify type):__________________________________ Date of Last Seizure: ______________ |
|||
________________________________ |
_______________________________ |
_________________ |
|
Name of Physician (please print) |
Physician’s Signature |
|
Date |
Physician Address: _____________________________________________ |
Physician Phone Number: ____________________________ |
||
12/11/09, revised 7/24/12
Documents used along the form
The Annual Physical Examination form is a crucial document for assessing an individual's health status. Several other forms and documents often accompany it to ensure comprehensive care and accurate record-keeping. Below is a list of these related documents.
- Medical History Form: This form collects detailed information about a patient's past medical history, including previous illnesses, surgeries, and family health history.
- Medication List: A comprehensive list of all medications a patient is currently taking, including dosages and prescribing doctors, helps prevent drug interactions and ensures safe treatment.
- Motor Vehicle Bill of Sale: This essential document records the sale of a vehicle between a buyer and seller, serving as a receipt for the transaction and proof of ownership transfer. To learn more, visit https://toptemplates.info/bill-of-sale/motor-vehicle-bill-of-sale.
- Immunization Record: This document tracks all vaccinations a patient has received, which is important for assessing immunity and planning future vaccinations.
- Consent for Treatment: Patients must sign this form to give healthcare providers permission to perform medical procedures or treatments during their visit.
- Lab Test Orders: These orders specify any laboratory tests needed during the physical examination, such as blood tests or urinalysis, and are essential for diagnosing health issues.
- Referral Form: If a specialist's evaluation is needed, this form is used to refer the patient to another healthcare provider for further assessment or treatment.
- Insurance Information Form: This document collects details about a patient's insurance coverage, which is necessary for billing and reimbursement purposes.
- Patient Registration Form: New patients typically complete this form to provide their personal information, including contact details and emergency contacts.
- Advance Directive: This form outlines a patient's preferences for medical treatment in case they become unable to communicate their wishes in the future.
- Follow-Up Care Plan: After the examination, this document outlines any recommended follow-up appointments, tests, or lifestyle changes based on the findings of the physical exam.
Each of these documents plays a vital role in ensuring that healthcare providers have the necessary information to deliver effective and personalized care. Proper completion and organization of these forms can help streamline the healthcare process for both patients and providers.