Free Do Not Resuscitate Order Template
When it comes to end-of-life care, the Do Not Resuscitate (DNR) Order form plays a crucial role in ensuring that individuals receive the medical treatment they desire—or do not desire—during critical moments. This document allows patients to express their wishes regarding resuscitation efforts in the event of cardiac arrest or respiratory failure. It is essential for patients to understand that a DNR order does not mean a refusal of all medical care; rather, it specifies that no aggressive measures, such as chest compressions or intubation, should be taken to revive them if they stop breathing or their heart stops beating. The form must be completed and signed by a qualified healthcare provider, and it often requires the consent of the patient or their legal representative. Understanding the implications of a DNR order is vital, as it can significantly impact the quality of care and the emotional well-being of both patients and their families during challenging times. By clarifying these wishes ahead of time, individuals can ensure that their preferences are honored, allowing for a more peaceful and dignified end-of-life experience.
Do Not Resuscitate Order - Adapted for State
Key takeaways
Filling out a Do Not Resuscitate (DNR) Order form is an important decision for individuals and their families. Here are key takeaways to consider:
- Understand the Purpose: A DNR order informs medical personnel that a patient does not wish to receive cardiopulmonary resuscitation (CPR) in the event of cardiac arrest.
- Consult with Healthcare Providers: Discuss your wishes with doctors or healthcare professionals. They can provide guidance and help clarify any questions.
- Discuss with Family: Open communication with family members is crucial. Ensure they understand your wishes and the implications of a DNR order.
- Complete the Form Accurately: Fill out the DNR order form carefully. Ensure all required information is provided to avoid confusion during emergencies.
- Sign and Date: The form must be signed and dated by the patient or their legal representative to be valid.
- Keep Copies Accessible: Store copies of the DNR order in easily accessible places, such as with your medical records or at home.
- Inform Medical Personnel: Make sure that your healthcare providers and emergency contacts are aware of the DNR order and its location.
- Review Regularly: Revisit your DNR order periodically, especially if your health status or preferences change.
- Understand State Laws: Be aware that DNR laws can vary by state. Familiarize yourself with local regulations to ensure compliance.
Making informed choices about a DNR order can provide peace of mind for you and your loved ones.
Guide to Writing Do Not Resuscitate Order
Completing a Do Not Resuscitate (DNR) Order form is an important step in ensuring that your healthcare preferences are respected. After filling out the form, it is advisable to keep a copy for your records and share it with your healthcare provider, family members, and anyone else involved in your care. This ensures that your wishes are clearly understood and can be followed when necessary.
- Obtain a copy of the Do Not Resuscitate Order form from your healthcare provider or an authorized source.
- Read the instructions carefully to understand the information required.
- Fill in your full name, date of birth, and other identifying information as requested.
- Indicate your preferences regarding resuscitation clearly on the form.
- Sign and date the form to validate your wishes.
- Have a witness sign the form, if required by your state laws.
- Make copies of the completed form for your records.
- Provide copies to your healthcare provider and family members.
Other Forms:
How Many Pages Does a Passport Have - Lost passports require immediate reporting to prevent identity theft.
The process of buying or selling a vehicle in North Carolina requires careful attention to detail, and having the proper documentation is essential. One integral piece of this process is the Motor Vehicle Bill of Sale form, which provides a clear record of the transaction, ensuring that both parties are protected and that all necessary information regarding the sale is documented appropriately.
Childcare Receipt Template - Parents should ensure that each detail is filled out before concluding payment.
Form Preview Example
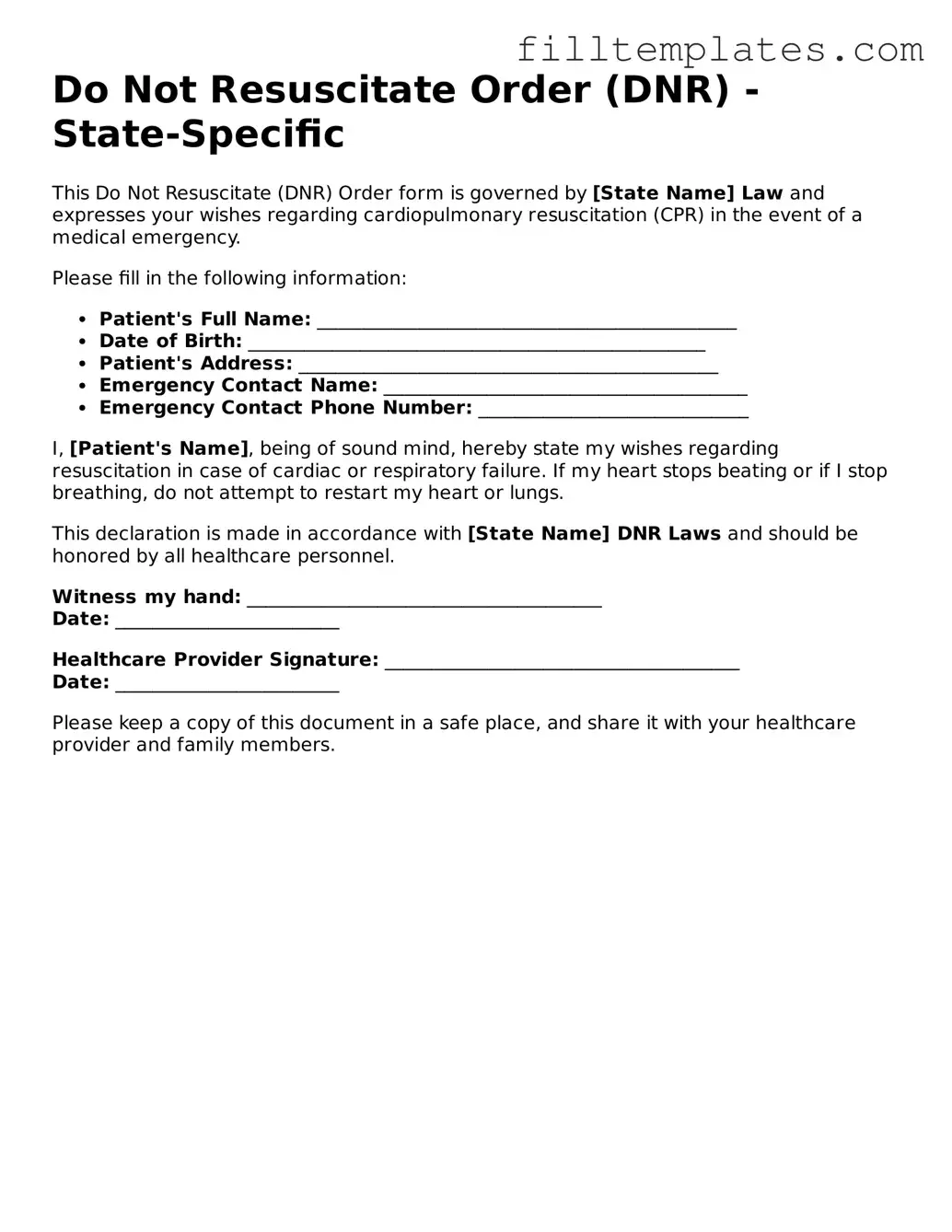
Do Not Resuscitate Order (DNR) - State-Specific
This Do Not Resuscitate (DNR) Order form is governed by [State Name] Law and expresses your wishes regarding cardiopulmonary resuscitation (CPR) in the event of a medical emergency.
Please fill in the following information:
- Patient's Full Name: _____________________________________________
- Date of Birth: _________________________________________________
- Patient's Address: _____________________________________________
- Emergency Contact Name: _______________________________________
- Emergency Contact Phone Number: _____________________________
I, [Patient's Name], being of sound mind, hereby state my wishes regarding resuscitation in case of cardiac or respiratory failure. If my heart stops beating or if I stop breathing, do not attempt to restart my heart or lungs.
This declaration is made in accordance with [State Name] DNR Laws and should be honored by all healthcare personnel.
Witness my hand: ______________________________________
Date: ________________________
Healthcare Provider Signature: ______________________________________
Date: ________________________
Please keep a copy of this document in a safe place, and share it with your healthcare provider and family members.
Documents used along the form
A Do Not Resuscitate (DNR) Order is an important legal document that communicates a patient's wishes regarding resuscitation efforts in the event of cardiac or respiratory arrest. However, several other forms and documents often accompany a DNR order to ensure comprehensive healthcare planning and decision-making. Below is a list of these documents, each serving a distinct purpose in the context of patient care.
- Advance Healthcare Directive: This document allows individuals to outline their preferences for medical treatment in situations where they may be unable to communicate their wishes. It can include specific instructions about various types of care, not limited to resuscitation.
- Healthcare Power of Attorney: This legal instrument designates a specific person to make healthcare decisions on behalf of the patient if they become incapacitated. The appointed agent can make choices consistent with the patient's values and preferences.
- Living Will: A living will is a type of advance directive that explicitly states a person's wishes regarding life-sustaining treatments in terminal or irreversible conditions. It may address issues such as artificial nutrition and hydration.
- Physician Orders for Life-Sustaining Treatment (POLST): This document translates a patient's treatment preferences into actionable medical orders. It is often used for patients with serious illnesses and provides clear guidance to healthcare providers.
- Do Not Intubate (DNI) Order: Similar to a DNR, a DNI order specifically instructs medical personnel not to insert a breathing tube in the event of respiratory failure. This document focuses on airway management rather than cardiac resuscitation.
- Patient Identification and Information Forms: These forms collect essential information about the patient, including medical history and current medications. They help healthcare providers make informed decisions about treatment options.
- Medication Administration Records: These records track the medications administered to a patient, including dosages and times. They are crucial for ensuring that treatment aligns with the patient's wishes and medical needs.
- Emergency Medical Services (EMS) Protocols: These guidelines inform emergency responders about a patient's DNR status and other critical medical information. They ensure that the patient's wishes are respected in emergency situations.
- Employment Verification Form: This document is essential for confirming the employment status of individuals and often contains key information such as job title and salary details, making it particularly useful during loan applications and background checks. For more information, visit OnlineLawDocs.com.
- Patient Consent Forms: These documents secure consent for various medical procedures and treatments. They affirm that the patient understands the potential risks and benefits of the proposed interventions.
In summary, while a Do Not Resuscitate Order is a vital component of end-of-life planning, it is typically accompanied by several other documents that collectively provide a comprehensive view of a patient's healthcare preferences. Understanding these forms can facilitate better communication among patients, families, and healthcare providers, ensuring that individual wishes are honored throughout the medical care process.