Download Tb Test Template
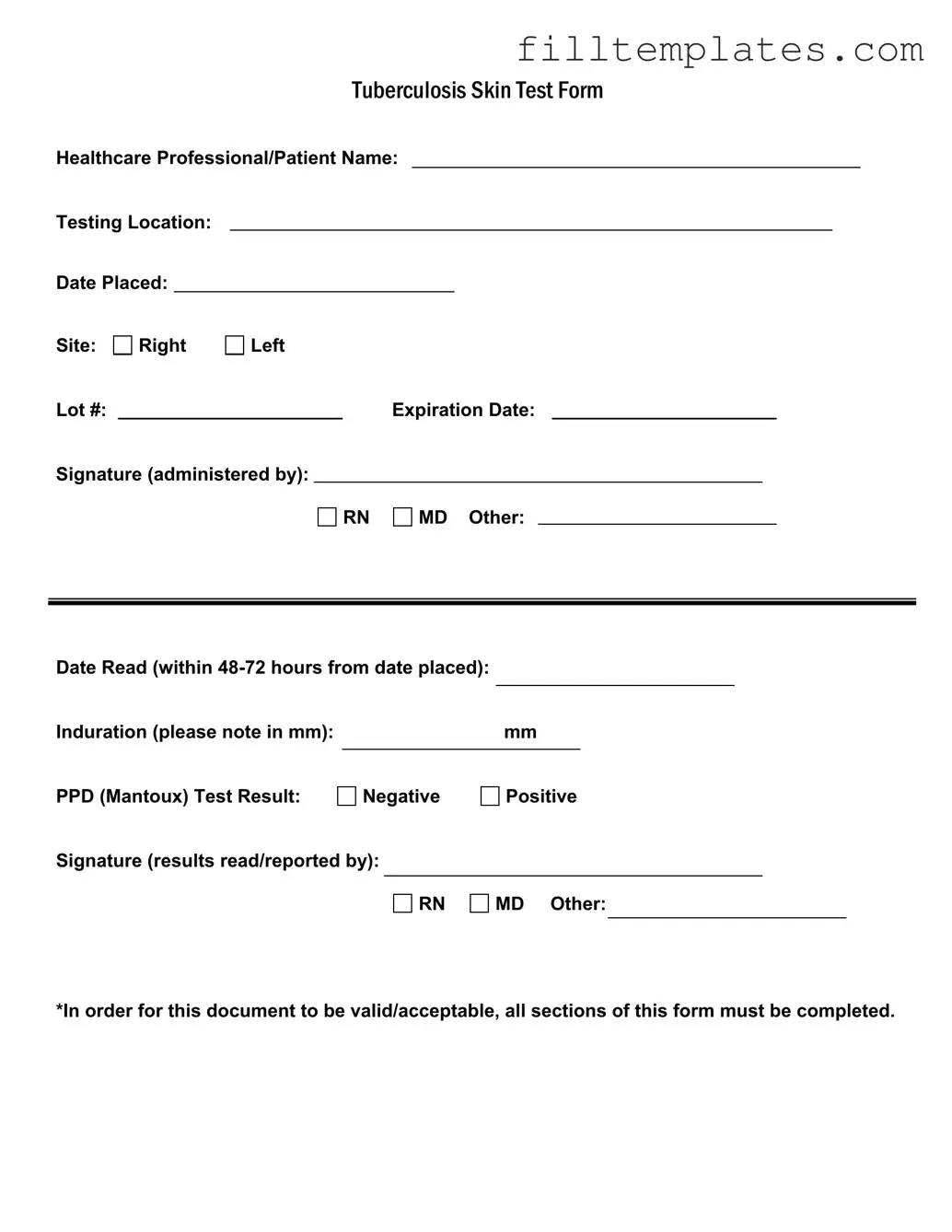
The Tuberculosis (TB) Skin Test form is a crucial document used in the assessment of tuberculosis exposure and infection. This form requires the name of the healthcare professional administering the test and the patient's name, ensuring clear identification of both parties involved. It also specifies the testing location and the date the test was placed, which is essential for tracking the timeline of the assessment. The site of the test is indicated as either the right or left arm, and it includes important details such as the lot number and expiration date of the testing material. To validate the test, the administering professional, whether a registered nurse (RN) or a medical doctor (MD), must sign the form. Additionally, the form requires a date when the test results are read, which must occur within 48 to 72 hours of placement. The induration measurement, recorded in millimeters, indicates the body's reaction to the test, while the PPD (Mantoux) test result is clearly marked as either negative or positive. Finally, the results must be confirmed with another signature from a qualified professional, ensuring that all sections of the form are completed for it to be valid and acceptable.
Key takeaways
When filling out and using the TB Test form, several key points should be kept in mind to ensure accuracy and compliance.
- Complete All Sections: It is essential that every section of the form is filled out. An incomplete form may not be accepted.
- Accurate Identification: Clearly write the healthcare professional's name and the patient's name to avoid confusion.
- Testing Location: Specify where the test is being conducted. This information is vital for record-keeping.
- Date Placed: Record the exact date when the test was administered. This is important for tracking and follow-up.
- Induration Measurement: Measure the induration in millimeters accurately. This result is crucial for interpreting the test outcome.
- Timely Reading: The test must be read within 48 to 72 hours. Ensure that the date read is noted on the form.
- Signature Requirement: The form must include signatures from the administering professional and the person reading the results. This adds validity to the document.
By following these guidelines, individuals can ensure that the TB Test form is filled out correctly and is ready for submission or record-keeping.
Guide to Writing Tb Test
Once you have the TB Test form, it is essential to fill it out accurately. This form requires specific information to ensure it is valid and acceptable. Follow these steps carefully to complete the form.
- Write the name of the healthcare professional or patient at the top of the form.
- Fill in the testing location where the TB test will be administered.
- Enter the date the test is placed.
- Indicate the site of the test by marking either "Right" or "Left."
- Record the lot number of the test.
- Note the expiration date of the test.
- The healthcare professional administering the test should sign the form and indicate their title (RN, MD, or Other).
- After 48-72 hours, the test must be read. Fill in the date the test is read.
- Measure and note the induration in millimeters (mm).
- Mark the PPD (Mantoux) test result as either "Negative" or "Positive."
- The healthcare professional reading the results should sign the form and indicate their title (RN, MD, or Other).
Make sure all sections of the form are completed to ensure it is valid. Double-check your entries for accuracy before submitting the form.
Browse Other PDFs
Make a Gift Card - Can be a great way to introduce new products or services.
In addition to serving as vital evidence of a vehicle transaction, the Texas Motor Vehicle Bill of Sale form can often be conveniently accessed online, such as through resources like smarttemplates.net, which provide fillable templates to simplify the process for both buyers and sellers.
Membership Certificate Template - A record of membership interests issued and transferred within a company.
Form Preview Example
|
|
|
|
|
TUBERCULOSISSKINTESTFORM |
||||||||
Healthcare Professional/Patient Name: |
|||||||||||||
Testing Location: |
|
|
|
|
|
|
|
|
|
|
|
||
Date Placed: |
|
|
|
|
|
|
|
|
|
|
|
|
|
Site: |
Right |
Left |
|
|
|
|
|
|
|
|
|||
Lot #: |
|
|
|
|
|
Expiration Date: |
|
|
|||||
Signature (administered by): |
|
|
|
|
|
|
|
|
|
||||
|
|
|
|
|
RN |
|
MD Other: |
|
|
|
|||
Date Read (within |
|
|
|
|
|
|
|
Induration (please note in mm): |
|
mm |
|
PPD (Mantoux) Test Result: |
|
|
|
Negative |
Positive |
||
Signature (results read/reported by):
RN
MD Other:
*In order for this document to be valid/acceptable, all sections of this form must be completed.
Documents used along the form
When dealing with tuberculosis testing, several other forms and documents often accompany the TB Test form. Each of these documents serves a specific purpose, ensuring that patients receive comprehensive care and that their health records are properly maintained. Below is a list of commonly used forms alongside the TB Test form.
- Patient Consent Form: This document obtains the patient’s permission to conduct the TB test. It outlines the procedure, potential risks, and benefits, ensuring that patients are informed before proceeding.
- Medical History Questionnaire: This form collects relevant health information from the patient. It may include past illnesses, current medications, and any previous TB exposure, helping healthcare providers assess the patient's risk factors.
- Referral Form: If a patient requires further testing or specialist consultation, this form facilitates the referral process. It typically includes patient details, the reason for the referral, and any relevant medical history.
- Results Notification Form: After the TB test results are available, this document informs the patient of their results. It may also include instructions for follow-up care based on the outcome.
- Motorcycle Bill of Sale Form: This form is significant for motorcycle transactions in California, ensuring a legal record of ownership transfer. For more information, visit https://toptemplates.info/bill-of-sale/motorcycle-bill-of-sale/california-motorcycle-bill-of-sale/.
- Immunization Record: This form tracks the patient's vaccination history, which may be relevant for assessing overall health and determining if additional immunizations are needed.
- Follow-Up Care Plan: If the TB test results are positive, this document outlines the necessary steps for further evaluation and treatment. It ensures that patients receive appropriate care promptly.
- Billing Information Form: This form collects insurance and payment information from the patient. It ensures that the healthcare provider can process claims and manage costs related to the TB test and any subsequent care.
- Patient Education Materials: These materials provide information about tuberculosis, its transmission, and prevention strategies. They are essential for helping patients understand their condition and how to protect themselves and others.
Each of these documents plays a crucial role in the overall process of tuberculosis testing and care. By ensuring that all necessary forms are completed and understood, healthcare providers can offer the best possible support to their patients.